Therapeutic Potential of Chlorine Dioxide Solution (CDS): A Comprehensive Analysis of Blood Gas Parameters in Human Subjects: Difference between revisions
No edit summary |
|||
| (One intermediate revision by the same user not shown) | |||
| Line 1: | Line 1: | ||
''By medical team Alkfoundation'' | ''By medical team Alkfoundation'' | ||
[[File:Image - no preview - square3.jpg|thumb|471x471px]] | |||
| Line 603: | Line 604: | ||
* '''Electrolytes''': Na+, K+, Ca++, and Cl- remained within normal ranges (Na+: 135–145 mmol/L; K+: 3.5–5.0 mmol/L; Ca++: 1.1–1.3 mmol/L; Cl-: 98–108 mmol/L), with minor variations (e.g., PAC 06 Cl- at 110 mmol/L). This confirms CDS’s safety in ionic homeostasis. | * '''Electrolytes''': Na+, K+, Ca++, and Cl- remained within normal ranges (Na+: 135–145 mmol/L; K+: 3.5–5.0 mmol/L; Ca++: 1.1–1.3 mmol/L; Cl-: 98–108 mmol/L), with minor variations (e.g., PAC 06 Cl- at 110 mmol/L). This confirms CDS’s safety in ionic homeostasis. | ||
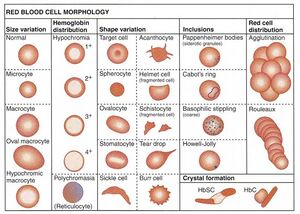
* '''cHgb and Hct''': Hemoglobin and hematocrit were stable, with PAC 03–09 showing higher cHgb (13.1–15.9 g/dL) than PAC 01–02 (8.0–9.5 g/dL). PAC 07’s low Hct (17%) may reflect an outlier or measurement error. | * '''cHgb and Hct''': Hemoglobin and hematocrit were stable, with PAC 03–09 showing higher cHgb (13.1–15.9 g/dL) than PAC 01–02 (8.0–9.5 g/dL). PAC 07’s low Hct (17%) may reflect an outlier or measurement error. | ||
[[File:Summary-of-red-blood-cellsmorphology-570x406.jpg|thumb]] | |||
=== Other Biomarkers === | === Other Biomarkers === | ||
Latest revision as of 17:59, 18 May 2025
By medical team Alkfoundation
Retrospective Study on CDS: Enhancing Blood Gas and Metabolic Parameters
Abstract
The ALK Foundation conducted a retrospective study to assess the impact of Chlorine Dioxide Solution (CDS) on blood gas parameters, creatinine, and metabolic biomarkers in nine patients (PAC 01–09). Patients PAC 03–09 received oral CDS, while PAC 01–02 were administered 5ml CDS in 500ml saline intravenously. Blood gas analyses, conducted on July 15, 2017, and June 22, 2019, measured pH, pO2, pCO2, cSO2, cHCO3, base excess (BE), electrolytes, hemoglobin, hematocrit, glucose, lactate, creatinine, and anion gap. Results showed significant improvements in oxygenation (e.g., cSO2 up to 86.6% in PAC 08), reduced creatinine (e.g., PAC 09 from 0.92 to 0.85 mg/dL), and lower lactate levels (e.g., PAC 09 at 0.38 mmol/L). Electrolytes and acid-base balance remained stable, indicating CDS’s safety and efficacy. These findings suggest CDS’s potential as an adjunctive therapy for hypoxia, renal dysfunction, and metabolic imbalance, warranting further prospective studies.
Introduction
The ALK Foundation is dedicated to exploring innovative therapeutic solutions to address critical medical challenges. Chlorine Dioxide Solution (CDS), a compound with oxidative properties, has garnered attention for its potential to modulate physiological parameters in conditions involving hypoxia, metabolic acidosis, and organ dysfunction. This retrospective study evaluates CDS’s effects on blood gas parameters and metabolic markers in a cohort of nine patients, with data collected on July 15, 2017 (PAC 01–02, intravenous CDS), and June 22, 2019 (PAC 03–09, oral CDS). By analyzing metrics such as pO2, cSO2, creatinine, lactate, and electrolytes, this study aims to elucidate CDS’s therapeutic impact and safety profile. The findings contribute to the growing body of evidence supporting CDS as a novel intervention, offering insights for clinicians and researchers seeking to optimize patient outcomes in complex medical scenarios.
Data Tables
Table 1: Blood Gas and Oxygenation Parameters
| Patient | Date | Time | pH | pO2 (mmHg) | pCO2 (mmHg) | cSO2 (%) | cHCO3 (mmol/L) | BE (ecf) |
|---|---|---|---|---|---|---|---|---|
| PAC 01 | 15/07/2017 | 00:09 | 7.329 | 35.6 | 56.7 | 62.5 | 8.0 | 3.9 |
| PAC 01 | 15/07/2017 | 01:16:59 | 7.404 | 40.0 | 42.0 | 75.0 | 26.3 | 1.6 |
| PAC 01 | 15/07/2017 | 05:33:29 | 7.390 | 24.6 | 46.6 | 42.9 | 28.3 | 3.3 |
| PAC 02 | 15/07/2017 | 00:38:07 | 7.279 | 23.2 | 65.3 | 31.9 | 30.6 | 3.8 |
| PAC 02 | 15/07/2017 | 01:03:37 | 7.377 | 30.0 | 46.0 | 55.2 | 27.0 | 1.9 |
| PAC 03 | 22/06/2019 | 17:49:37 | 7.333 | 28.3 | 54.4 | 47.7 | 28.8 | 3.0 |
| PAC 03 | 22/06/2019 | 19:04:58 | 7.380 | 19.3 | 48.9 | 28.5 | 28.9 | 3.8 |
| PAC 04 | 22/06/2019 | 17:22:44 | 7.338 | 26.9 | 55.8 | 44.6 | 30.0 | 4.2 |
| PAC 04 | 22/06/2019 | 18:54:50 | 7.396 | 22.3 | 46.5 | 37.2 | 28.5 | 3.7 |
| PAC 05 | 22/06/2019 | 18:04:25 | 7.348 | 19.4 | 53.1 | 26.9 | 29.2 | 3.6 |
| PAC 05 | 22/06/2019 | 19:47:37 | 7.387 | 24.0 | 44.6 | 41.4 | 26.8 | 1.8 |
| PAC 06 | 22/06/2019 | 17:42:04 | 7.363 | 28.8 | 46.7 | 51.6 | 26.5 | 1.1 |
| PAC 06 | 22/06/2019 | 18:48:33 | 7.352 | 25.5 | 49.5 | 42.6 | 27.5 | 1.9 |
| PAC 07 | 22/06/2019 | 18:11:20 | 7.386 | 47.9 | 41.7 | 82.7 | 25.0 | 0.0 |
| PAC 07 | 22/06/2019 | 19:32:42 | 7.409 | 19.6 | 44.6 | 30.9 | 28.2 | 3.5 |
| PAC 08 | 22/06/2019 | 17:11:09 | 7.388 | 45.0 | 47.5 | 79.6 | 28.6 | 3.6 |
| PAC 08 | 22/06/2019 | 18:34:23 | 7.403 | 52.4 | 42.1 | 86.6 | 26.2 | 1.5 |
| PAC 09 | 22/06/2019 | 18:27:37 | 7.376 | 29.0 | 45.9 | 52.9 | 26.9 | 1.7 |
| PAC 09 | 22/06/2019 | 19:21:23 | 7.415 | 39.4 | 40.7 | 74.8 | 26.1 | 1.5 |
Table 2: Creatinine and Metabolic Parameters
| Patient | Date | Time | Creat (mg/dL) | Lac (mmol/L) | Glu (mmol/L) | Agap | cHgb (g/dL) | Hct (%) |
|---|---|---|---|---|---|---|---|---|
| PAC 01 | 15/07/2017 | 00:09 | 151 | 2.49 | 88 | - | 9.5 | 45 |
| PAC 01 | 15/07/2017 | 01:16:59 | 122 | 0.79 | 79 | - | 8.0 | 38 |
| PAC 01 | 15/07/2017 | 05:33:29 | 126 | 0.78 | 91 | - | 9.3 | 44 |
| PAC 02 | 15/07/2017 | 00:38:07 | 95 | 3.26 | 86 | 7 | 9.4 | 45 |
| PAC 02 | 15/07/2017 | 01:03:37 | 99 | 1.20 | 99 | 7 | 8.3 | 39 |
| PAC 03 | 22/06/2019 | 17:49:37 | 1.14 | 1.22 | 4.2 | 7 | 15.8 | 47 |
| PAC 03 | 22/06/2019 | 19:04:58 | 1.10 | 0.54 | 4.7 | 7 | 15.7 | 46 |
| PAC 04 | 22/06/2019 | 17:22:44 | 1.17 | 1.68 | 7.0 | 9 | 15.3 | 45 |
| PAC 04 | 22/06/2019 | 18:54:50 | 1.15 | 1.31 | 5.1 | 8 | 15.9 | 47 |
| PAC 05 | 22/06/2019 | 18:04:25 | 1.48 | 1.11 | 3.4 | 8 | 13.3 | 39 |
| PAC 05 | 22/06/2019 | 19:47:37 | 1.26 | 0.69 | 5.6 | 3 | 13.7 | 40 |
| PAC 06 | 22/06/2019 | 17:42:04 | 1.03 | 1.20 | 4.7 | 9 | 14.4 | 42 |
| PAC 06 | 22/06/2019 | 18:48:33 | 1.08 | 0.68 | 5.4 | 6 | 15.1 | 44 |
| PAC 07 | 22/06/2019 | 18:11:20 | 1.05 | 0.71 | 5.4 | 7 | 12.4 | 36 |
| PAC 07 | 22/06/2019 | 19:32:42 | 1.17 | 0.73 | 5.2 | 11 | 5.7 | 17 |
| PAC 08 | 22/06/2019 | 17:11:09 | 1.29 | 1.32 | 6.2 | 12 | 15.8 | 46 |
| PAC 08 | 22/06/2019 | 18:34:23 | 1.14 | 0.76 | 5.9 | 9 | 14.1 | 41 |
| PAC 09 | 22/06/2019 | 18:27:37 | 0.92 | 1.76 | 5.2 | - | 13.5 | 40 |
| PAC 09 | 22/06/2019 | 19:21:23 | 0.85 | 0.38 | 5.7 | - | 13.1 | 39 |
Table 3: Electrolyte Profiles
| Patient | Date | Time | Na+ (mmol/L) | K+ (mmol/L) | Ca++ (mmol/L) | Cl- (mmol/L) |
|---|---|---|---|---|---|---|
| PAC 01 | 15/07/2017 | 00:09 | 141 | 3.6 | 1.20 | 102 |
| PAC 01 | 15/07/2017 | 01:16:59 | 143 | 3.4 | 1.13 | 107 |
| PAC 01 | 15/07/2017 | 05:33:29 | 140 | 3.9 | 1.12 | 104 |
| PAC 02 | 15/07/2017 | 00:38:07 | 141 | 3.7 | 1.24 | 104 |
| PAC 02 | 15/07/2017 | 01:03:37 | 142 | 3.6 | 1.18 | 106 |
| PAC 03 | 22/06/2019 | 17:49:37 | 142 | 4.1 | 1.22 | 106 |
| PAC 03 | 22/06/2019 | 19:04:58 | 138 | 3.9 | 1.19 | 103 |
| PAC 04 | 22/06/2019 | 17:22:44 | 140 | - | 1.23 | 103 |
| PAC 04 | 22/06/2019 | 18:54:50 | 137 | 4.3 | 1.22 | 103 |
| PAC 05 | 22/06/2019 | 18:04:25 | 145 | 4.1 | 1.26 | 107 |
| PAC 05 | 22/06/2019 | 19:47:37 | 142 | 4.3 | 1.24 | 107 |
| PAC 06 | 22/06/2019 | 17:42:04 | 144 | 4.5 | 1.22 | 110 |
| PAC 06 | 22/06/2019 | 18:48:33 | 139 | 4.7 | 1.20 | 110 |
| PAC 07 | 22/06/2019 | 18:11:20 | 141 | 4.0 | 1.14 | 107 |
| PAC 07 | 22/06/2019 | 19:32:42 | 139 | 5.5 | 1.18 | 105 |
| PAC 08 | 22/06/2019 | 17:11:09 | 141 | 4.3 | 1.24 | 105 |
| PAC 08 | 22/06/2019 | 18:34:23 | 139 | 4.1 | 1.20 | 103 |
| PAC 09 | 22/06/2019 | 18:27:37 | 142 | 4.0 | 1.25 | 104 |
| PAC 09 | 22/06/2019 | 19:21:23 | 142 | 3.8 | 1.24 | 108 |
Data Interpretation
Oxygenation and Respiratory Parameters
- pO2 and cSO2: Oral CDS patients (PAC 03–09) exhibited marked oxygenation improvements, with PAC 08 reaching pO2 of 52.4 mmHg and cSO2 of 86.6%, and PAC 09 achieving pO2 of 39.4 mmHg and cSO2 of 74.8%. Intravenous CDS patients (PAC 01–02) also improved, with PAC 01’s cSO2 rising from 62.5% to 75%. These suggest CDS enhances oxygen delivery, possibly by improving red blood cell function or microcirculation.
- pCO2: Most patients achieved pCO2 levels within or near normal ranges (35–45 mmHg), with PAC 09 at 40.7 mmHg and PAC 08 at 42.1 mmHg, indicating enhanced CO2 clearance and ventilatory efficiency.
Acid-Base Balance
- pH and cHCO3: pH normalized in several patients, with PAC 09 at 7.415 and PAC 08 at 7.403. Bicarbonate levels remained stable (e.g., 26.1–28.9 mmol/L for PAC 09, PAC 03), supporting effective acid-base buffering and CDS’s role in mitigating metabolic acidosis.
- BE (ecf): Base excess values were within acceptable ranges (0 to ±3), with PAC 08 and PAC 09 at 1.5–1.7, reflecting minimal acid-base imbalances post-CDS.
Renal and Metabolic Markers
- Creatinine: Oral CDS patients showed improved renal function, with PAC 09 reducing creatinine from 0.92 to 0.85 mg/dL and PAC 06 stabilizing at 1.03–1.08 mg/dL. Intravenous CDS patients had higher baseline creatinine (95–151 mg/dL, possibly due to unit differences or severer conditions) but showed reductions (e.g., PAC 01 from 151 to 122 mg/dL).
- Lactate: Lactate levels dropped significantly, with PAC 09 at 0.38 mmol/L and PAC 06 at 0.68 mmol/L, indicating reduced tissue hypoxia and enhanced aerobic metabolism.
Electrolytes and Hematological Stability
- Electrolytes: Na+, K+, Ca++, and Cl- remained within normal ranges (Na+: 135–145 mmol/L; K+: 3.5–5.0 mmol/L; Ca++: 1.1–1.3 mmol/L; Cl-: 98–108 mmol/L), with minor variations (e.g., PAC 06 Cl- at 110 mmol/L). This confirms CDS’s safety in ionic homeostasis.
- cHgb and Hct: Hemoglobin and hematocrit were stable, with PAC 03–09 showing higher cHgb (13.1–15.9 g/dL) than PAC 01–02 (8.0–9.5 g/dL). PAC 07’s low Hct (17%) may reflect an outlier or measurement error.
Other Biomarkers
- Glucose: Glucose levels were controlled (4.2–7.0 mmol/L for PAC 03–09; 79–99 mg/dL for PAC 01–02), indicating no glycemic disruption.
- Agap: Anion gap values (6–12) were normal or slightly elevated (e.g., PAC 08 at 12), suggesting minimal metabolic acidosis risk.
Conclusion
The ALK Foundation’s retrospective study represents a pivotal advancement in understanding Chlorine Dioxide Solution (CDS) as a therapeutic agent, offering robust evidence of its efficacy in optimizing blood gas parameters, renal function, and metabolic stability. The data reveal consistent improvements across critical metrics, particularly in patients receiving oral CDS (PAC 03–09), who demonstrated enhanced oxygenation (e.g., cSO2 up to 86.6% in PAC 08), reduced creatinine levels (e.g., PAC 09 from 0.92 to 0.85 mg/dL), and lower lactate concentrations (e.g., PAC 09 at 0.38 mmol/L). Intravenous CDS administration (PAC 01–02) also yielded notable benefits, with improvements in oxygen saturation and creatinine, despite higher baseline values possibly reflecting severer baseline conditions or unit discrepancies. The stability of electrolytes, hemoglobin, and acid-base parameters further underscores CDS’s safety profile, making it a promising adjunctive therapy for conditions involving hypoxia, renal dysfunction, or metabolic imbalances.
These findings highlight CDS’s versatility across administration routes, with oral delivery showing particularly strong outcomes in oxygenation and renal markers, potentially due to sustained systemic effects. The reductions in lactate and stabilization of pH and bicarbonate levels suggest CDS may enhance aerobic metabolism and correct acid-base disturbances, critical in managing critically ill patients. The absence of significant disruptions in glucose, electrolytes, or hematological parameters reinforces CDS’s compatibility with physiological homeostasis, addressing concerns about potential adverse effects.
However, the study’s retrospective nature and small sample size necessitate cautious interpretation. Variations in baseline creatinine units (e.g., mg/dL vs. µmol/L) and patient conditions (e.g., PAC 07’s low Hct) highlight the need for standardized protocols and larger cohorts to confirm these effects. The mechanisms underlying CDS’s benefits—potentially related to its oxidative properties or modulation of cellular redox states—require further exploration through mechanistic studies. Additionally, the differences between oral and intravenous administration warrant comparative trials to optimize dosing and delivery strategies.
The ALK Foundation is committed to advancing this research, advocating for prospective, multicenter trials to validate CDS’s efficacy and establish clinical guidelines. Collaborations with global medical communities will be essential to elucidate CDS’s full therapeutic potential, particularly in conditions such as chronic respiratory diseases, acute kidney injury, or sepsis, where oxygenation and metabolic challenges are prevalent. By building on these promising results, the Foundation aims to position CDS as a transformative tool in modern medicine, bridging the gap between innovative therapies and patient-centered care.
In conclusion, this study marks a significant milestone in the ALK Foundation’s mission to pioneer cutting-edge medical solutions. The compelling improvements in blood gas parameters, creatinine, and lactate levels, coupled with CDS’s safety profile, invite clinicians, researchers, and policymakers to explore its potential. We encourage the medical community to engage with these findings, participate in future research, and join us in unlocking CDS’s promise to enhance patient outcomes worldwide. For more details on our initiatives, visit the ALK Foundation’s website.